INTRODUCING
THERANOSTICS
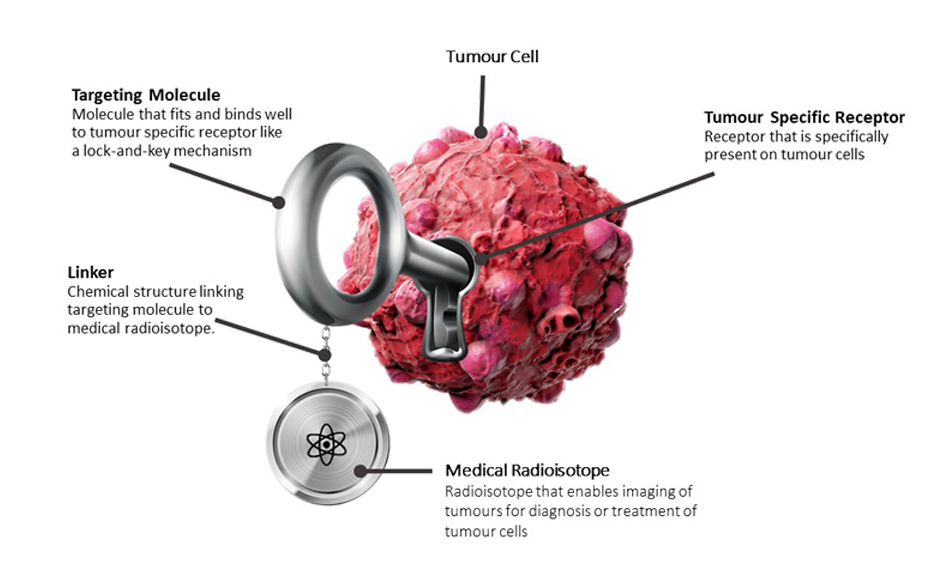
Theranostics is a novel therapeutic paradigm which combines specific targeted therapy based on diagnostic molecular imaging. Theranostics is an approach which focuses on patient centred care and is a significant leap ahead from the conventional medicine to precision medicine.
ABOUT THERANOSTICS
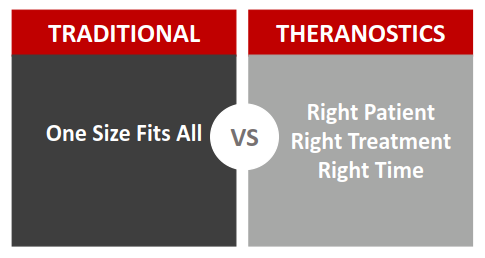
Traditional cancer treatment plan works through the one-size-fits-all medicine model. In such model, patients are given standard treatment and subsequently, follow-ups are carried out to evaluate patient’s response to the treatment and if the outcome is undesirable, a different treatment will be started.
Theranostics is a novel therapeutic paradigm that is part of the growing field of personalized medicine. It utilizes the pairing of molecular imaging and radioligand therapy (RLT), allowing for effective diagnosis, therapy and subsequent treatment monitoring, therefore enhancing the efficacy of treatment and quality of care to the patient.
Radionuclides used for molecular imaging are radioactive materials that are either used on their own or more commonly tagged with a drug or peptide molecule in small quantities to image bones, organs and other parts of the body. Depending on the part of the body that is targeted, different radioactive material is used to acquire the images. These images are acquired either with a SPECT scanner or a PET scanner and when combined with CT imaging technology, high quality images can be acquired to enable physician to identify the primary and metastatic cancer cells in the body and to predict if patient could benefit from the paired radioligand therapy. As the targeting ligand used for the molecular imaging is the same or very similar to that of the radioligand therapy, the prediction of treatment outcome is highly precise, sparing patient from unnecessary side effects and cost of ineffective treatment.
Radioligand therapy is a precision medicine treatment option available for the treatment of cancer. Therapeutic radionuclides, similar to their diagnostic counterparts, are either used on their own or tagged to a drug or peptide. To achieve the cytotoxic effect necessary to destroy tumour cells, radioactive dose administered is higher compared to diagnostic imaging. As a principle of precision medicine, radioligand therapy employs a targeted approach which minimizes collateral damage to surrounding healthy cells.
THERANOSTICS APPLICATIONS

Prostate Cancer
Prostate Cancer occurs in the cells of the prostate gland which play a part in the male reproductive system. Typically prostate cancer cells are slow-growing but once it begins to metastasize, it could be life-threatening.

Neuroendocrine Tumours
Neuroendocrine Tumors (NETs) are tumours originated from the hormone-producing cells or nerve cells (the neuroendocrine system). There are many kinds of NETs but they are all group as one due to the similar features and characteristics of the cells.

Thyroid Cancer
Thyroid cancer occurs in the cells of the thyroid gland which plays a part in production of hormones that regulates the heart rate, blood pressure, body temperature and weight. Different types of thyroid cancer manifest different symptoms in patients. The use of radioiodine on thyroid cancer patients is one of the longest-existing theranostics applications.
What is PSA?
PSA is an abbreviation for Prostate-Specific Antigen which is a protein that is produced in the prostate gland. It can be found in the circulating bloodstream at elevated levels in men with prostate cancer. The PSA level is one of several tools used to monitor disease progression and treatment efficacy in prostate cancer patients.
What is PSMA?
PSMA is Prostate-Specific Membrane Antigen (PSMA) which is an antigen that is highly expressed in prostate cancer cells. In recent years, there has been many studies on using PSMA-ligand for diagnostics and treatment of prostate cancer. These studies have shown promising results for the patients with advance prostate cancer (mCRPC).
Why is it important and how it works?
As PSMA is highly expressed in over 90% of prostate cancers, researchers have designed imaging ligands that would bind to PSMA in the body. With such PSMA-ligands that are labelled with Gallium-68 (Ga-68) and systemically introduced into the patient body, clinicians are able to track the expression of PSMA in the body (ie. the metastatic sites of the prostate cancer) through PET/CT imaging system. Such images provide very useful tumour localization information that will allow clinicians to perform more accurate treatment plan, ensuring the right treatment is given to the right patient at the right stage of the disease.
When a radioligand therapy (RLT) is recommended, the same PSMA-ligands used during PET/CT imaging, will also be used at therapeutic doses to kill the metastasized prostate cancer cells. However, instead of labelling the PSMA-ligands with imaging isotopes like Ga-68 or Fluorine-18, it is labelled with therapeutic isotopes such as Lutetium-177 (Lu-177) or Actinium-225 (Ac-225). Lu-177 or Ac-225 labelled PSMA-ligands would absorb to the same location as that of Ga-68 labelled PSMA-ligands, thus, enabling the specific sites seen on the images during diagnosis stage to be treated precisely.
When does your patient need a PSMA PET scan?
The Ga-68-PSMA-ligands scan can be recommended for your patients with confirmed prostate cancer such as patients with high PSA level, positive CT/MRI/bone scans and/or histological results from biopsy. The scans are also very often done on patients with biochemical recurrence of prostate cancer who has previously undergone surgery or radiotherapy as well as some primary staging of prostate cancer.
Who could benefit from Lu-177-PSMA-ligand therapy?
Lu-177-PSMA-ligands therapy is a form of radioligand therapy which may be recommended by the clinicians should there be positive uptake of Ga-68-PSMA-ligands from the PET/CT scans.
Early clinical studies have demonstrated positive response with Lu-177-PSMA-ligand therapy in many of the patients who have already failed other therapies. Although many of the published studies have shown very promising efficacy of the treatment using Lu-177-PSMA-ligands therapy, it is noteworthy that most of these studies were evaluated in end stage prostate cancer patients. Theoretically, Lu-177-PSMA-ligands therapy could be more effective in early stage prostate cancer when the lesions are small, however, such data is yet to be available.

Rasul, S. et al. Eur J Nucl Med Mol Imaging 47, 713–720 (2020). Article is licensed by http://creativecommons.org/licenses/by/4.0/
The above Kaplan-Meier plot shows the median overall survival and median progression-free survival among a study cohort of 54 patients. Patients received 3 cycles of highly standardized Lu177-PSMA RLT at 4-weekly intervals. The median overall survival was 119 weeks and the median progression-free survival was 25 weeks

Rasul, S. et al. Eur J Nucl Med Mol Imaging 47, 713–720 (2020). Article is licensed by http://creativecommons.org/licenses/by/4.0/
Remarkable lesion resolution in Ga-68 PSMA PET/CT after completing 3 cycles of Lu-177 PSMA RLT. Ga-68 PSMA images of mCRPC patients before and after 3 cycles of Lu-177 PSMA RLT: (a) patient with therapy response and PSA drop of about 70% (initial PSA 80.95 µg/L, after therapy PSA 22.95 µg/L); the arrows indicate residual metastatic areas. (b) Patient with therapy response and PSA decline of >80% (initial PSA 70.68 µg/L, after therapy PSA 6.4 µg/L)
ASSISTANCE
For clinicians who wish to obtain more information about providing the above imaging and treatment options to your patient, please CONTACT US.
What is Somatostatin Receptor (SSTR)?
Somatostatin (SST) is a hormone that is produced by the body to regulate our body’s endocrine system which includes organs such as pituitary gland, thyroid gland, parathyroid glands, adrenal glands, pancreas, ovaries and testicles. Somatostatin Receptors (SSTR) are cellular receptor that SST binds to in order to perform their regulatory function.
Why is it important and how it works?
SSTR are found to be over-expressed in Neuroendocrine Tumours (NETs). This is an important factor because the over-expression allows the tumour cells to be targeted specifically, thus enabling a non-invasive approach to precisely image the disease and perform personalized therapy. Common somatostatin analogues peptide tracers that are used to target over-expressed SSTR are DOTATATE, DOTATOC and DOTANOC.
Imaging
DOTATATE is an SST analogue that behaves similarly to the SST that our body produce, it therefore binds to the SSTR that are over-expressed by NET. By coupling DOTATATE with a small amount of radioactive isotope such as Indium-111 (In-111) or Gallium-68 (Ga-68), a SPECT or PET scan respectively can be performed to capture a precise image of the localization of the tumour lesions anywhere in the body, size of the tumour lesions and the extend of metastases (if any). The information obtained from the scan images enables clinician to better recommend appropriate treatment options and monitor the efficacy of on-going treatment.
Therapy
When DOTATATE is coupled to a therapeutic isotope such as Lutetium-177 (Lu-177), the specificity of the SST analogue brings a therapeutic dose of radiation into to the tumour cell. Radiation induces DNA strands to break, resulting in tumour cells death killing the tumour cells at the primary and metastasized sites.The over-expression of SSTR in NET is advantageous as it allows the radioactive Lu-177 -DOTATATE to accumulate in the tumour lesions and limit off-site binding. Clinical studies have shown encouraging clinical responses such as shrinkage of tumour, improvement in the quality of life and longer survival following therapy with the radioactive isotope Lu-177. Patients with high uptake in their diagnostic Ga-68 DOTATATE/ DOTATOC/ DOTANOC PET scan or In-111 Octreoscan SPECT scan typically respond better to the Lu-177 therapy targeting somatostatin receptors with well tolerated side effects.
When does your patient need a SST PET or SPECT scan?
Adult patients with confirmed or suspected well-differentiated Gastroenteropancreatic-Neuroendocrine tumours (GEP-NETs) for the purpose of diagnosis, staging, therapy planning and dosimetry.
Who could benefit from the Lu-177 STT Therapy?
The therapy is most often administered for Gastroenteropancreatic- Neuroendocrine tumours (GEP-NETs) that have positive expression of SSTR in the gastro-entero-pancreatic (GEP) and bronchial tracts, but may also include patients with phaeochromocytoma, paraganglioma, neuroblastoma or medullary thyroid carcinoma.
ASSISTANCE
For clinicians who wish to obtain more information about providing the above imaging and treatment options to your patient, please CONTACT US.
What is Radioiodine (I-131)?
Radioiodine is the first theranostic radionuclide in nuclear medicine history which is used for diagnostic and therapy of thyroid disease. Oral administration of radioiodine either capsule or liquid has been used to treat thyroid cancer and benign thyroid conditions for more than 40 years. I-131 is a gamma (364 keV) and beta emitter (average 192 keV, max 606keV) where the emission of beta energy is used for therapy and the emission of gamma is used for scintigraphy imaging with the gamma camera/SPECT.
Why is it important and how it works?
The major role of radioiodine for thyroid cancer are:
a. Ablation of the thyroid remnant and existing functional metastases post thyroidectomy
b. Diagnosis of recurrences
c. Treatment of recurrent disease
Iodine is an essential part of our diet– our body requires small amounts of iodine to produce thyroid hormones essential to growth and development. When either form of iodine is introduced into the body, it accumulates in the thyroid gland. Thus, radioactive iodine has been used to treat thyroid cancer. Radioiodine is absorbed by the thyroid remnant (post thyroidectomy) and metastases site. The beta energy from the radioiodine will deposit into the thyroid remnant (post thyroidectomy) and metastases site, thus, killing them.
Thyroid cancer is a common and often curable malignancy. There are 4 type of thyroid cancers - Papillary, Follicular, Medullary and Anaplastic. Papillary thyroid cancer is the most common thyroid cancer. Both papillary thyroid cancer and follicular thyroid cancers are classified as well-differentiated thyroid cancer. Medullary and Anaplastic thyroid cancer are rare. Radioiodine is only used to treat well-differentiated thyroid cancer – Papillary and Follicular.
When does your patient need Radioiodine scans?
Radioiodine scans, which are done using either a gamma camera or a SPECT scanner, is typically performed for clinicians to study the radioiodine kinetics and to estimate the thyroid uptake of patients who have elevated thyroid hormones in their blood.
Clinicians may recommend a low dose Radioiodine whole-body scan with SPECT to evaluate residual thyroid tissue from post thyroidectomy and to determine any metastases for thyroid cancer patients.
Who could benefit from Radioiodine therapy?
Radioiodine therapy is for treatment of Graves disease, toxic multinodular goitre, autonomous nodules, papillary and follicular thyroid carcinoma.Radioiodine is often combined with surgical intervention and with antithyroid medications. On Day-3 or Day-4 post radioiodine treatment, whole-body scan with gamma camera or SPECT is performed to evaluate the distribution of the radioiodine and to determine any metastases and the progression of the disease.
ASSISTANCE
For clinicians who wish to obtain more information about providing the above imaging and treatment options to your patient, please CONTACT US.
Actinium-225 (Ac-225) is an alpha emitting radioisotope with a half-life of 10 days. The primary decay path of Ac-225 yields a total of 4 energetic alpha particles. Alpha particles have short travel distance and high linear energy transfer, in clinical context; this means that the alpha particles can deliver a highly cytotoxic dose of radiation to targeted cells while minimizing collateral damage to non-targeted cells.
Ac-225 therapy is the use of the radioisotope Ac-225 in conjunction with a suitable targeting agent, such as a PSMA-ligand, to specifically target and kill tumour cells. PSMA-ligands such as PSMA I&T are selected for their selectivity and specificity in targeting prostate cancer cells. When PSMA I&T is tagged with Ac-225, it allows the radioactive Ac-225 molecule to be brought to the prostate cancer cells where the cytotoxic radiation emitted then kills the cancer cell. The short effective range of the alpha particles emitted minimizes harm to the healthy cells nearby, and therefore, reducing potential side effects.
An initial study of Ac-225 PSMA therapy has reported a PSA decline of > 90% in 82% of study cohort (17 patients) and 88% of patients with >50% decline in lesions avidity as imaged by Ga68-PSMA-PET/CT including 11 patients with complete resolution (1). Various other studies have also similarly demonstrated the effective anti-tumour activity of Ac-225 therapy (2)(3) with xerostomia as the primary side effect.

Fig. 1 a: Waterfall plot showing PSA response at 8 weeks after one cycle of 225Ac-PSMA-617 radioligand therapy. b: Waterfall plot showing best PSA response to 225Ac-PSMA-617 radioligand therapy

Fig 2: A treatment-naïve patient who presented with extensive bone metastasis at primary diagnosis achieved a complete remission after three cycles of 225Ac-PSMA-617 with de-escalating activities of 8/7/6 MBq (patient number 16)
Similar to other radioisotopes, the cytotoxic radiation emitted by Ac-225 can be harnessed for treatment of other diseases. When tagged to a PSMA-ligand, Ac-225 is used in prostate cancer therapy and when tagged with a somatostatin analog, Ac-225 can be used for treatment of Neuroendocrine tumors (NETs). Ac-225 has also been applied in a conditioning regime prior to bone marrow transplant in patients with Acute Myeloid Leukemia (AML) and results from clinical trial thus far have been positive. As new targeting agents for various diseases are developed, Ac-225 will continue to be an option to complement them.
Ac-225 therapy is currently used either in research or when standard of care treatment fails to deliver an effective and lasting response. In the latter case, Ac-225 therapy is used (compassionate use) to overcome resistance to, beta radiation, gamma radiation, chemotherapeutic drugs and hormone drugs. Clinical trials are underway to provide formal data on treatment efficacy and safety profile of Ac-225 therapies and when successful, a wider group of patients would be able to benefit from the availability of an effective alternative therapy.
Empowering you to provide cutting-edge
therapies to your cancer patients
QT Instrument has been in the business of providing turnkey solutions to hospitals, clinics and laboratories since 1994. We constantly source for new effective
therapies, and equip our clients with the tools, technology, environment
and trainings needed for them to deliver quality services to their patients.
Our Services

Facility Setup for In-house Preparation and Dispensing of Radiopharmaceuticals

Radiation Facility QV&V Services

Radioactive Waste Management Solutions

Radioiodine Ward Design and Setup

Training and Consultation Services

Customized Solutions for Safe Radiation Handling and Transportation

Customized Nuclear Medicine and PET Laboratories
We design and customize laboratories and equipment to ensure our clients’ facility is well-equipped to deliver high quality patient care and services in an efficient, safe and compliant manner.
CONTACT US
Our Theranostics Clients
We study and make careful consideration of our clients’ passion, vision and mission, and
provide consultation and solutions to enable our clients to achieve them
effectively and efficiently.

Nuclear Medicine and PET Centres

Radiopharmacy Laboratories

GMP Cyclotron Facilities

R&D Radiochemistry Laboratories
Our Reference Centres
Lutetium-177 Radioligand Therapy (RLT) is one of the therapeutic isotopes used in theranostics. It has gained much attention in the recent years due to the development of new and effective targets for precision medicine especially in prostate cancer and neuroendocrine tumours (NETs).
Lu-177 RLT is currently available in Singapore, Malaysia and Thailand. If you wish to find out about the medical centres offering such therapy, please CONTACT US.

2016
YEAR
INTRODUCED
12
NUMBER OF CENTRES
IN SEA
>3000
DIAGNOSTIC IMAGING
PERFORMED IN SEA
>800
RADIOLIGAND
THERAPY
PERFORMED
If excellent patient care is at your heart…
